Despite relentless efforts to curb tuberculosis (TB) in Nigeria, the disease continues to claim thousands of lives annually. The World Health Organization (WHO) 2022 Global TB report shows that Nigeria has the highest burden of TB in Africa and ranks sixth globally. The country has an incidence of 219 per 100,000 population.
This public health crisis is compounded by two major factors: ignorance and poverty.
With over 40 percent of the population living below the poverty line, the link between deprivation and TB is undeniable. Poverty not only fuels TB transmission but also perpetuates the disease’s devastating cycle. It traps vulnerable communities in a loop where the illness thrives, leading to financial ruin, stigma, and death.
Ignorance and traditional beliefs
Low awareness and misconceptions about TB significantly hinder early diagnosis and treatment. Many people attribute their symptoms to spiritual causes, relying on traditional healers rather than seeking medical attention. These beliefs are deep-rooted and persistent, particularly in rural areas where formal healthcare services are scarce.
Take Abdusalam Abdulquadri, a survivor of drug-resistant TB (DRTB) for instance, He endured nine months of severe illness, trying various herbal remedies and seeking spiritual solutions, believing his condition was caused by a spiritual attack. It wasn’t until his health deteriorated further, and he began coughing up blood, that his family took him to a hospital. After numerous tests, he was diagnosed with DRTB and placed on a grueling treatment regimen.
Abdulquadri recalls, “My ignorance nearly cost me my life. I thought it was a spiritual attack, and I wasted months trying different herbs before seeking medical help. It was only by the grace of God that I survived.
“My ordeal began five years ago while studying at the National Open University in Abeokuta. I had persistent chest pains. Initially, I dismissed it as minor discomfort, but it worsened over time. Despite trying various remedies, including herbal treatments and self-medication, my condition deteriorated.
“I developed a severe cough, isolated myself and eventually began coughing up blood. Fearful of a spiritual attack, I sought help from a herbalist in Ijebu Ode. However, traditional remedies proved ineffective. My health declined rapidly, and I was on the brink of despair. With the support of my family, I finally sought medical attention.
“After undergoing tests, I was diagnosed with DRTB. The subsequent treatment was arduous, with intense side effects and a demanding medication regimen. Despite the challenges, I survived with the unwavering support of my loved ones,” Abdulquadri said.
Poverty: A catalyst
Poverty worsens the challenges of battling TB. While the treatment for TB is free at government-supported DOTS centers, the associated costs, transportation, nutritional needs, and time away from work become overwhelming for many. Abdullahi Musa, a 45-year-old mechanic from Kano, exemplifies this struggle.
Living in a densely populated area with poor sanitation and limited healthcare access, Abdullahi initially ignored his symptoms, assuming they were caused by exhaustion from work. Like many others in his community, he didn’t associate his cough, weight loss and night sweats with TB. It was only when herbal treatments failed, and his health severely declined, that he sought professional care. By then, his TB had worsened, and the costs of transportation to the health center, coupled with his reduced income from missed work, became insurmountable.
For Abdullahi, the financial burden meant skipping doses of his medication, which only prolonged his illness and put his family at risk of infection.
Stigma
In addition to poverty and ignorance, stigma remains a significant barrier to treatment. Many TB patients face discrimination from their communities and even healthcare providers.
Mrs. Kadiri Oluseyi, another TB survivor living with HIV, experienced this firsthand. She recalls the stigma she faced from health providers and her community. “People would avoid me because of my illness. The stigma was overwhelming, and at one point, I stopped taking my medication altogether because of the way I was treated,” she says. Her experience is not unique; stigma often forces TB patients into isolation, further delaying treatment and increasing the risk of spreading the disease.
Expert opinions
Coordinator of the Civil Society for the Eradication of TB, Olayide Akanni, while speaking recently at the media training for Journalist on TB and Tuberculosis Preventive Treatment (TPT) organised by Journalists Against AIDS and supported by Treatment Action Group, TAG, highlighted the critical role ignorance and poverty play in fueling TB in Nigeria.
She said: “Awareness campaigns need to emphasize that TB is curable, and treatment is free. We need to combat the spiritual and traditional misconceptions surrounding TB and encourage people to seek proper medical care early.”
Akanni believes that media engagement is crucial in spreading TB awareness.
“The media has a broad reach, and it’s essential that we use it to educate the public about TB symptoms, treatment options, and the fact that TB is curable. We also need to address the socio-economic barriers that prevent people from accessing treatment, such as transportation costs and nutrition.”
Also, Mrs. Stella Makpu, from the National Tuberculosis, Leprosy, and Buruli Ulcer Control Program, emphasized the importance of awareness in tackling tuberculosis.
Common misconceptions
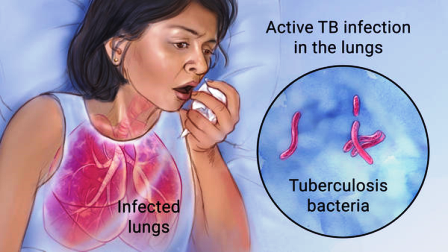
Makpu stated that TB is not caused by witchcraft, a curse from the gods, or a generational curse. Not everyone who has TB also has HIV, and it is neither hereditary nor incurable. On how TB is transmitted, she said, “TB germs are released into the air when a person with TB of the lungs, especially those not on appropriate treatment, coughs or sneezes. A healthy person can become infected with TB when he breathes in the TB germs.”
She highlighted the six-month Directly Observed Treatment Therapy (DOT), stressing that patients must complete the full course to avoid complications.
“If treatment is cut short, drug-resistant TB can develop, which is much harder to treat.” She also discussed preventive therapies, including various drug regimens to stop the spread of TB, especially after contact tracing.
Breaking the cycle
To effectively combat TB, addressing both poverty and ignorance is essential. Public health campaigns need to focus on educating communities about TB symptoms, transmission, and treatment. Additionally, financial support programs to alleviate the costs of accessing healthcare, along with nutritional support for TB patients, are critical.
Without tackling these root causes, TB will continue to devastate Nigeria’s most vulnerable communities. TB is curable, but only if the barriers of ignorance, poverty, and stigma are broken.